As more and more patients seek care for pelvic floor dysfunction, the need for more qualified practitioners is becoming apparent. Many patients prefer to see a clinician who they identify with, which is why it is important for practitioners of all genders to learn to treat pelvic floor dysfunction. Because much of the public's awareness of pelvic rehab comes out of women's health, the vast majority of pelvic health practitioners are women.
There is currently a shortage of male pelvic health practitioners. To help us understand why it is so important to fix that, we reached out to several male clinicians who have attended the Male Pelvic Floor: Function, Dysfunction, and Treatment course to ask them about the need for more men in the field. Here are some answers to the question:
“Why is it important to have male providers available to treat male patients in the field of pelvic health?”
Grant Headley of Bridgetown Physical Therapy of Portland, Oregon (www.bridgetownpt.com)
While as PT’s we all approach our patients with interest in helping them as individuals, some of our patients feel more comfortable sharing certain details with a provider of the same gender. Many of the hang-ups some men have about receiving care from a female provider are related to an older generation, to certain traditional or religious cultural beliefs, or to certain beliefs about propriety related to receiving care.
As acknowledged in our coursework, generally men have cultural barriers that traditionally do not permit sharing of vulnerability or weakness, especially in the sexual domain. Here are a few unsolicited statements I feel encapsulate what my own male patients have told me: Some heterosexual men feel more comfortable sharing the details of their dysfunction with a man because they find it difficult to admit vulnerability in the presence of a female. Some men prefer not to relay the clinically pertinent details of dysfunctional sexual encounters with a female because they do not wish to make the female practitioner uncomfortable. Many men feel that they can relay more detail about the mechanics of the sexual dysfunction or signs of improvement to a male provider. Some men have told me that they felt their sexual dysfunction was minimized or that they have been treated with patronizing language by a female pelvic PT in the past. Unfortunately, these patients attribute this negative experience to the PT being female, and they are not comfortable having a second opinion with a female.
 Although we strive to present as open-minded and neutral to our patients, they may have an affinity for a male provider. This could foster a more constructive clinical partnership towards working on their goals if they perceive fewer communication barriers. I can offer my own experience as a past patient suffering with pelvic floor dysfunction; I was so desperate for help and I felt so grateful that there was a physical therapist in my city at all that was willing to help me. I did not care that she was female and that I had to receive treatment at a women's health clinic for new mothers in the University Hospital. Many female therapists reading this article have likely transferred lifesaving PT care to scores of men. This organization of H&W that does so much good for a sensitive aspect of men's care is dominated by women- this needs to be acknowledged as a net positive but also appreciated that much of the education and application of care is an adaptation from what has worked for women in the past. Many men will be so grateful to receive care and get better. Some men unfortunately will have barriers to receiving care and for those patients, we can seek out and encourage our male colleagues to get involved in pelvic rehab so we can all provide more access to care.
Although we strive to present as open-minded and neutral to our patients, they may have an affinity for a male provider. This could foster a more constructive clinical partnership towards working on their goals if they perceive fewer communication barriers. I can offer my own experience as a past patient suffering with pelvic floor dysfunction; I was so desperate for help and I felt so grateful that there was a physical therapist in my city at all that was willing to help me. I did not care that she was female and that I had to receive treatment at a women's health clinic for new mothers in the University Hospital. Many female therapists reading this article have likely transferred lifesaving PT care to scores of men. This organization of H&W that does so much good for a sensitive aspect of men's care is dominated by women- this needs to be acknowledged as a net positive but also appreciated that much of the education and application of care is an adaptation from what has worked for women in the past. Many men will be so grateful to receive care and get better. Some men unfortunately will have barriers to receiving care and for those patients, we can seek out and encourage our male colleagues to get involved in pelvic rehab so we can all provide more access to care.
Lance Frank of Flex Physical Therapy in Atlanta (www.flexptatl.com)
Personally, as a male provider in pelvic health, I find that the men I treat are much more comfortable and at ease discussing topics like erections (or lack thereof) and sexual dysfunction, as well as incontinence, or pelvic pain. In a female dominated sub-specialty of physical therapy, sometimes as a male it can be intimidating and even embarrassing for some men to discuss these topics at all, let alone with a female; so having the option to speak and be treated by another male who may better understand the changes, anatomy, and problems they’re experiencing may feel a bit less daunting. Our culture has made male masculinity fragile and I think some populations of men who need pelvic floor rehab may feel embarrassed to be treated by a female clinician if their perception of being seen by a female is emasculating. Ultimately, I think there needs to be more men in this field because there needs to be better visibility of male pelvic health providers in general, as well as better representation of men acknowledging that male pelvic floor disorders exist and are willing and able to treat them.
Eddie Gordon of Flow Rehab in Seattle (www.flowrehab.com)
There are far fewer male physiotherapists treating men with pelvic floor dysfunctions, but I am hopeful this will change for the better. Lack of access to male pelvic physios is a relative barrier to care because some men are more comfortable seeing a male pelvic provider the same way most women would prefer seeing a female pelvic physio. In general, men do not typically seek treatment as frequently or early enough the way most women do. If male pelvic physios are not available, then men may more likely delay treatment, which could potentially worsen their problem. Ironically, when it comes to men with pelvic floor dysfunctions, men are underrepresented, but I am hopeful that more male PT’s will be joining the movement to educate the male population.
Milan Patel of Comprehensive Therapy Services in San Diego (comprehensivetherapy.com)
I believe it's important to have male providers in the pelvic health field for many reasons, one being the opportunity for connection. I think we connect best with reflections of ourselves and for men seeking out a pelvic health provider that can be hard to find. In my experience, pelvic physical therapy works best when your patient can be open and honest, and establishing a strong connection between therapist and patient is the first step. Another reason is that people should have options for the provider they want. In San Diego I am the only male pelvic physical therapy provider which means most men seeking pelvic floor therapy have no choice but to see a female. If you switched the genders in the last sentence you could see how that is problematic. Many women prefer to have their pelvic PT be a female, I just think guys should get the same choice.
Steven Lavender of The Physical Therapy Practice NYC in New York (thephysicaltherapypractice.nyc)
In my experience as a gay male practitioner practicing pelvic floor physio on only men:
Gay male patients usually prefer a gay provider because they feel like they don’t have to explain lifestyle issues and choices, they may be unused to being touched by women, and maybe misogynistic.
Some straight men have told me that they think a male practitioner would know more about their pelvic issues than a woman. Some men don’t think women are strong enough nor have long enough fingers to get to the places they need to be. Some straight men report they might be attracted to a female therapist and get an erection or feel embarrassed about appearing unmanly with their particular pelvic condition.
For some men being touched by a woman is a religious issue so many males of the Jewish and Muslim faiths prefer to see a male practitioner.
Some men could not care less who sees them as long as they get better.
One woman called me for advice or for an appointment from some distance because they "figured a gay man in New York City just might know more about my ass and ass pain than any local jack-assed doctor in my neck of the woods." True story.
If you are interested in learning to treat male patients, the Male Pelvic Floor: Function, Dysfunction, and Treatment course is a great place to start! The course is taking place twice more in 2019, this September 13-15, 2019 in Pasadena, CA, and again in Fort Myers, FL on October 19-21, 2019. We are already booked four times in 2020 as well, so be sure to check out the full course schedule for all available dates.
You have been treating a highly motivated 24-year-old woman with a diagnosis of Interstitial Cystitis/Painful Bladder Syndrome (IC/BPS). The plan of care includes all styles of manual therapy, including joint mobilization, soft tissue mobilization, visceral mobilization, and strain counterstrain. You utilize neuromuscular reeducation techniques like postural training, breath work, PNF patterns, and body mechanics. Your therapeutic exercise prescription includes mobilizing what needs to move and strengthening what needs to stabilize. Your patient is feeling somewhat better, but you know she has the ability to feel even more at ease in their day to day. Is there anything else left in the rehab tool box to use?
 Kanter et al. set out to discover if mindfulness-based stress reduction (MBSR) was a helpful treatment modality for (IC/BPS). The authors were interested in both the efficacy of a treatment centered on stress reduction and the feasibility of women adopting this holistic option.
Kanter et al. set out to discover if mindfulness-based stress reduction (MBSR) was a helpful treatment modality for (IC/BPS). The authors were interested in both the efficacy of a treatment centered on stress reduction and the feasibility of women adopting this holistic option.
The American Urological Association defined first-line treatments for IC/PBS to include relaxation/stress management, pain management and self-care/behavioral modification. Second-line treatment is pelvic health rehab and medications. The recruited patients had to be concurrently receiving first- and second-line treatments, and not further down the treatment cascade like cystoscopies and Botox.
The control group (N=11) received the usual care (as described above in first- and second-line treatments). The intervention group (N=9) received the usual care plus enrollment in an 8-week MBSR course based on the work of Jon Kabat- Zinn. The weekly course was two hours in the classroom supplemented with a 4-CD guide and book for home meditation practice carryover. The course content included meditation, yoga postures, and additional relaxation techniques.
The patients who participated in the MBSR program reported improved symptoms post-treatment, and perhaps more notably, their pain self-efficacy score (PSEQ) significantly improved. All but one of the participants reported feeling “more empowered” to control their bladder symptoms.
As clinicians working so intimately with our patients, we are often given the privilege of bearing witness to the emotional pain of healing chronic, persistent pelvic pain. We understand how terribly frightening it is for our patients to feel like they will never get better and we see this come out sometimes as fear-avoidance, which has the potential to cascade further into other areas of the social sphere.
If we are able to encourage holistic methods of building strategies to handle the challenges of IC/BPS, our patients will be set up for success in ways beyond the treatment room. While we hope for immediate results in the form of pain relief (which five patients in the study did), we also can appreciate the strategy building for resiliency in the face of persistent pain. As a very strong woman said, “hope serves us best when we do not attach specific outcomes to it”.
Dustienne Miller is the author and instructor of Yoga for Pelvic Pain. Join her in Manchester, NH on September 7-8, 2019 or in Buffalo, NY on October 5-6, 2019 to learn about treating interstitial cystitis/painful bladder syndrome, vulvar pain, coccydynia, hip pain, and pudendal neuralgia with a yoga approach.
Kanter G, Kommest YM, Qaeda F, Jeppson PC, Dunivan GC, Cichowski, SB, and Rogers RG. Mindfulness-Based Stress Reduction as a Novel Treatment for Interstitial Cystitis/Bladder Pain Syndrome: A Randomized Controlled Trial. Int Urogynecol J. 2016 Nov; 27(11): 1705–1711.
I recently found this article from the Psychology Research and Behavior Management Journal. I found myself curious about how other healthcare disciplines treat a diagnosis that often presents in conjunction with pelvic floor dysfunction. Irritable bowel syndrome, or IBS, affects nearly 35 million Americans. It is considered a ‘functional’ condition meaning that symptoms occur without structural or biochemical pathology. There is often a stigma with functional diagnosis that the symptoms are “all in their heads”, and while there are many theories about what predisposes individuals to IBS, the experts now think of IBS as a “disorder of gut brain interaction”. Generally, there are 3 subtypes of IBS where people note either constipation dominant, diarrhea dominant or mixed. In order to be diagnosed an individual must report abdominal pain at least 1 day per week in the last 3 months which is related to stooling and a change in frequency or form. Other symptoms that are common are bloating, nausea, incomplete emptying, and urgency.
The author suggests a biopsychosocial framework to help understand IBS. An interdependent relationship between biology (gut microbiota, inflammation, genes), behavior (symptom avoidance, behaviors), cognitive processes (“brain-gut dysregulation, visceral anxiety, coping skills”), and environment (trauma, stress). The brain-gut connection by a variety of nerve pathways is how the brain and gut communicate in either direction; top down or bottom up. Stress and trauma can dysregulate gut function and can contribute to IBS symptoms.
Stress affects the autonomic nervous system that contributes to sympathetic (fight/flight) and parasympathetic (rest/digest). Patients with IBS may have dysfunction with autonomic nervous system regulation. Symptoms of dysregulated gut function can present as visceral hypersensitivity, visceral sensitivity, and visceral anxiety. Visceral hypersensitivity is explained as an upregulation of nerve pathways. The author sites studies that note that IBS patients have a lower pain tolerance to rectal balloon distention than healthy controls. Visceral sensitivity is another sign of upregulation where IBS patients have a greater emotional arousal to visceral stimulation and are less able to downregulate pain. The author notes that the IBS population show particular patterns of anxiety with visceral anxiety and catastrophizing. Visceral anxiety is described hypervigilance to bowel movements and fear avoidance of situational symptoms. For example, fear of not knowing where the bathroom is located.
Cognitive behavioral therapy (CBT) has been shown to be an effective treatment to decrease the impact of IBS symptoms. CBT is focused on modifying behaviors and challenging dysfunctional beliefs. CBT can be presented in a variety of ways, however most include techniques consisting of education of how behaviors and physiology interplay for example the gut and stress response; relaxation strategies, usually diaphragmatic breathing and progressive relaxation; cognitive restructuring to help individuals see the relationship between thought patterns and stress responses; problem-solving skills with shift to emotion focused strategies (“acceptance, diaphragmatic breathing, cognitive restructuring, exercise, social support”) instead of problem focused strategies, and finally exposure techniques to help the individual slowly face fear avoidance behaviors. So much of the techniques are similar to what pelvic floor therapists try to educate our patients in. It is reassuring to me that through we may be different disciplines we are on the same team are moving towards the same goal. The author recommends a 10 session treatment duration, and notes that may be a barrier for some. Integrated practice with other healthcare professionals is also recommended. The more we can know about what our other team members are doing to help support patients the more effective we all are.
Kinsinger, Sarah W. “Cognitive-behavioral therapy for patients with irritable bowel syndrome: current insights” Psychology research and behavior management vol. 10 231-237. 19 Jul. 2017, doi:10.2147/PRBM. S120817
Ultrasound imaging is being used more frequently in the physical therapy clinical setting. Physical therapists are using ultrasound (US) imaging in varying ways. Some are using it as a training tool for the patient to learn neuromuscular control. Others are using it to guide needle placement while performing dry needling. In a recent article authored by several well-known physiotherapists, the various uses of US imaging were defined, as well as discussions regarding the scope of practice, and training for physiotherapists using ultrasound imaging.
 Four uses of US imaging have been reported by physical therapists. The first and most common use of US imaging is the evaluation of muscle structure and function to aid in neuromuscular control. Essentially, the US images are being used as a source of biofeedback. This has been coined Rehabilitative Ultrasound Imaging (RUSI). Additional uses have emerged in recent years including Diagnostic US imaging which is the diagnosis and monitoring of pathology; and interventional US imaging which is using the US images to guide percutaneous procedures involving dry or wet needling. These three categories are performed during clinical care and fall under the umbrella term “point of care ultrasound.” The last category of US imaging use in physical therapy is paired with performing research.
Four uses of US imaging have been reported by physical therapists. The first and most common use of US imaging is the evaluation of muscle structure and function to aid in neuromuscular control. Essentially, the US images are being used as a source of biofeedback. This has been coined Rehabilitative Ultrasound Imaging (RUSI). Additional uses have emerged in recent years including Diagnostic US imaging which is the diagnosis and monitoring of pathology; and interventional US imaging which is using the US images to guide percutaneous procedures involving dry or wet needling. These three categories are performed during clinical care and fall under the umbrella term “point of care ultrasound.” The last category of US imaging use in physical therapy is paired with performing research.
In this article, some thoughts and areas for improvement were brought to light regarding each type of US imaging as well as the scope of practice and training for each type of US use. It was mentioned that RUSI sits almost entirely within the scope of the physical therapy profession, however, it can be difficult for therapists to receive training for this use. Therapists interested in learning diagnostic or interventional US imaging have more options for training because these uses of US have established criteria for training, competence, and regulation outlined by the World Health Organization (WHO), as well as oversight from the World Federation for Ultrasound in Medicine and Biology. These programs often are intended for other healthcare practitioners (radiologists, and sonographers), but physical therapists are able to take the courses. However, it was stated that both diagnostic and interventional US imaging do not fall within the scope of practice for a majority of physical therapists around the world. So, although training may be more available for these types of US use; therapists taking these courses gain increased experience with non-physical therapy applications, and therefore are at risk for operating outside the scope of their practice.
The authors continued with distinct recommendations for needed training for the four different types of US imaging. Several of the listed skills were fundamental knowledge that a therapist should obtain before utilizing any of the four types of US into their practice such as basic physics for US, terminology, safety, among other knowledge. Then there were skills that were specific to the particular type of US being performed. Since point-of-care use of US is generally not included as part of entry level physical therapy education programs, this knowledge needs to be obtained in a postgraduate education format. For therapists who wish to learn diagnostic application of US imaging, there are multiple courses available from schools that train sonographers. However, according to this article, the form of US imaging that sits more within the scope of practice for physical therapists, rehabilitative ultrasound imaging, does not have as many educational opportunities as diagnostic US imaging does.
Herman & Wallace offers a course that provides fundamental skills of US imaging (such as history, and knowledge of the physics needed for US imaging), as well as specific skills for real-time ultrasound imaging. The schedule of the course includes a lot of lab time with multiple US units available so the ratio of participant to US unit low. You will leave the course being able to interpret US images and use it as an assessment tool or biofeedback tool for the patient. Using RUSI will change how you treat patients! The Rehabilitative Ultrasound Imaging course is offered three more times this year. Join me in Columbia, MO this August; Madison, WI in September; or Chicago, IL in December to learn how to use this form of ultrasound imaging in your clinical practice!
Whittaker J, Ellis R, Hodges P, et al. Imaging with ultrasound in physical therapy: what is the PT’s scope of practice a competency-based educational model and training recommendations. Br. J Sports Med. Apr. 2019; 0:1-7.
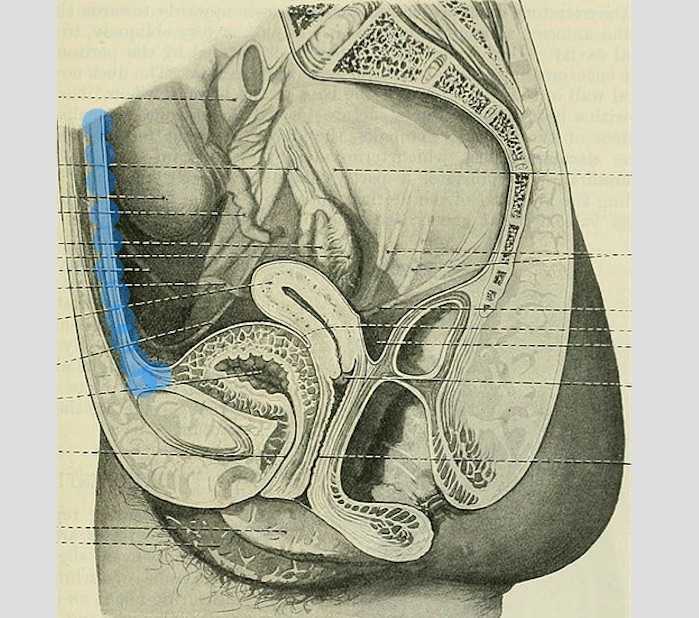
“However, at present we are all aglow with views on visceral anatomy and medical colleges are wisely establishing chairs in this department which will result in much advancement.” -Fred Byron Robinson, 1891 (Cysts of the Urachus)
The above (fabulous) quote reminds us that many came before us who were equally excited by the study of anatomy. One anatomical structure that I know never appeared in my graduate anatomy courses is the urachus. The urachus is a structure that extends from the urinary bladder to the umbilicus (highlighted blue in the image). When investigating literature about this structure I was impressed to find publications about the urachus dating from the late 19th century.
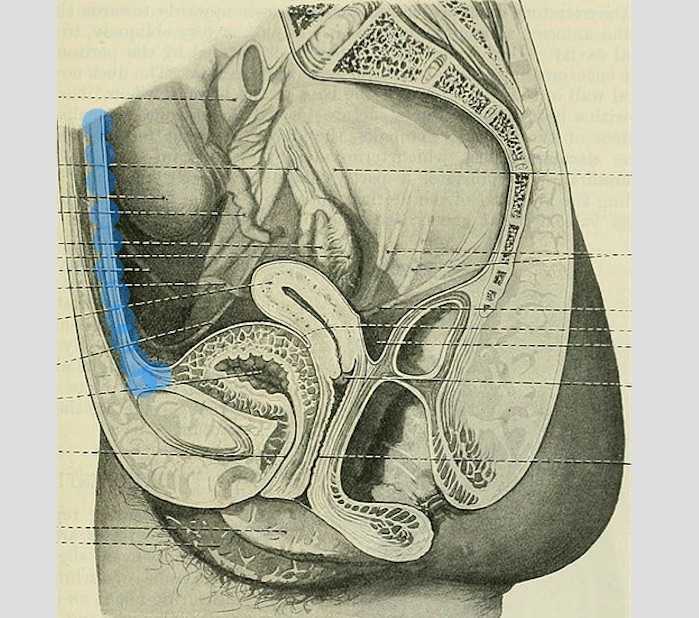
It wasn’t until several years into my career as a physical therapist that I learned about the urachus, a structure attached to the bladder, and learned how this structure could create some rather dramatic symptoms when in dysfunction. I met a woman who was in her early 30’s and who had 6 months prior undergone a laparoscopic surgery with access just below the umbilicus. She presented to rehabilitation after seeing an urologist for severe pain that occurred towards the end of voiding. The pain was absent at any other time, but was so severe towards the latter half of emptying her bladder that she would double over in pain and “nearly pass out.” Investigation revealed a healthy, well-functioning pelvic floor and abdominal wall, but a reproduction of her severe pain with palpation to the midline between the umbilicus and the pubic bone. After grabbing some anatomy texts, I supposed that the urachus, having potentially been irritated by the laparoscopic approach, might experience a tensioning of the irritated tissue as the bladder contracted to empty. This theory appeared to hold some weight, as applying gentle manual therapy to the tissues, and teaching the patient some self-release techniques allowed her to resolve her symptoms entirely after 1-2 visits.

The urachus is formed in early development from the pre-peritoneal layer, and is described as vestigial tissue. It extends from the anterior dome of the bladder to the umbilicus, varying in length from 3-10 cm, with a diameter of 8-10 mm. There are 3 layers: an inner layer of transitional or cuboid epithelial cells surrounded by a layer of connective tissue. The remains of the urachus form the middle umbilical ligament which is a fibromuscular cord. A layer of smooth muscle that is continuous with the detrusor (smooth muscle of the bladder) makes up the outer layer. This continuity of tissue may help explain some of the clinical connections we see in patient symptoms. In the past year, I have met several patients for whom the urachus is the only tissue that reproduced their symptoms. I examined a male patient who reported urethral burning that occurred with both reset and activity. Unable to produce symptoms in any other location of the thoracolumbar spine, pelvic floor and walls, or abdomen, I palpated this structure to find that it reproduced the urethral burning. Another patient presented with a keloid c-section scar. She also described a sharp pain when the bladder was full. Treatment directed to the scar and along the midline resolved this pain, again with a couple sessions.
If you are interested in learning more about distinct anatomical connections that can help you explain (and treat) issues your patients present with, come and learn with us at the 3-day Male Pelvic Floor Function, Dysfunction, and Treatment course offered four times over the 2019 and 2020 calendars. The role of the urachus in abdominopelvic dysfunction is just one of the many topics we explore. With lectures on sexual health, pelvic pain, prostate and urinary dysfunction, there is a broad range of topics and skills to offer for clinicians who are new to men’s heath and those who have been treating for years.
Begg, R. C. (1930). The Urachus: its Anatomy, Histology and Development. Journal of Anatomy, 64(Pt 2), 170–183.
Gray, H. (1918). Anatomy of the Human Body. Philadelphia: Lea & Febiger.
Sterling, J. A., & Goldsmith, R. (1953). Lesions of Urachus which Appear in the Adult. Annals of Surgery, 137(1), 120–128.
Most clinicians will agree that stress can amplify a patient’s pain and slow recovery. Mindfulness training provides patients with the ability to self-regulate their stress reaction and has been shown to reduce pain and depression and improve quality of life in patients with chronic pain conditions.1 The growing popularity of meditation training to manage stress has led to an increased interest in the physiological mechanisms by which meditation influences the body’s stress reaction. A systematic review and meta-analysis examined the results of randomized controlled trials that compared the impact meditation interventions to active control groups on stress measures. 2 Forty-five studies were included. Meditation practices examined were focused attention, open monitoring and mantra repetition. Outcome measures studied were cortisol, blood pressure, heart rate, lipid and peripheral cytokine expression. Studies had diverse participants including healthy adults, undergraduate students, army soldiers, veterans, cancer survivors, and individuals with chronic pain conditions, cardiovascular disease, depression and hypertension.
 When all meditation forms were analyzed together, meditation reduced blood cortisol, C-reactive protein, resting and ambulatory blood pressure, heart rate, triglycerides and tumor necrosis factor-alpha. The effect of meditation on:
When all meditation forms were analyzed together, meditation reduced blood cortisol, C-reactive protein, resting and ambulatory blood pressure, heart rate, triglycerides and tumor necrosis factor-alpha. The effect of meditation on:
- Cortisol and resting heart rate was considered to be high level of evidence.
- C-reactive protein, blood pressure, triglycerides and tumor necrosis factor-alpha was considered to be moderate level of evidence.
Analyzed individually:
- Open monitoring meditation reduced ambulatory systolic blood pressure, systolic blood pressure following a stress test and resting heart rate. Effects assessed as providing moderate level of evidence.
- Focused awareness reduced blood cortisol and resting systolic blood pressure. Effects assessed as providing low level of evidence.
- Mantra repetition reduced systolic blood pressure. Effects assessed as providing low level of evidence.
Authors report the primary reason for downgrading the grade of evidence when analyzing meditation practices individually was the limited number of studies available and small sample sizes. They conclude overall, when compared to an active control (relaxation, exercise or education) meditation practice leads to decreased physiological markers of stress in a range of populations.
Carolyn will offer her popular course, Mindfulness-Based Pain Treatment, in Portland OR, July 27 and 28 and again in Houston TX, October 26 and 27. We recommend these unique opportunities to train with Carolyn, a nationally recognized leader trailblazing the successful applications of mindfulness into pain treatment and the field of physical therapy. Hope to see you there!
1. Hilton L, Hempel S, Ewing BA, et al. Mindfulness meditation for chronic pain: Systematic review and meta-analysis. Ann Behav Med. 2017;51(2):199-213.
2. Pascoe MC, Thompson DR, Jenkins ZM, Ski CF. Mindfulness mediates the physiological markers of stress: Systematic review and meta-analysis. J Psychiatr Res. 2017;95:156-78.
Pain demands an answer. Treating persistent pain is a challenge for everyone; providers and patients. Pain neuroscience has changed drastically since I was in physical therapy school. This update comes from the International Spine and Pain Institute headed by the lead author Adriaan Louw, PT, PhD. If you are interested in reading more about persistent pain, I suggest reading the article in its entirety.
 This article brings together several comorbidities that pelvic physical therapists often encounter; fibromyalgia, chronic fatigue syndrome, irritable bowel syndrome, and chronic Lyme disease. The authors argue that all of these syndromes have many common symptoms and might be dependent on the provider that the individual goes to as to which diagnosis the individual receives. Often, once an individual has a diagnosis, he or she (more often she) then identifies with this label. The authors reason that once medical pathologies have been ruled out, then a more holistic, biopsychosocial approach may create better outcomes.
This article brings together several comorbidities that pelvic physical therapists often encounter; fibromyalgia, chronic fatigue syndrome, irritable bowel syndrome, and chronic Lyme disease. The authors argue that all of these syndromes have many common symptoms and might be dependent on the provider that the individual goes to as to which diagnosis the individual receives. Often, once an individual has a diagnosis, he or she (more often she) then identifies with this label. The authors reason that once medical pathologies have been ruled out, then a more holistic, biopsychosocial approach may create better outcomes.
Pain neuroscience education is a way to explain pain to patients, often with analogies, with a focus on neurobiology and neurophysiology as it relates to that individuals pain experience. To be able to educate our patients, we as providers, must be able to understand neuromatrix, output, and threat. Moseley states “[p]ain is a multiple system output activated by an individual’s specific pain neuromatrix. The neuromatrix is activated whenever the brain perceives a threat”. If that sounds like gibberish, consider watching this TEDx talk by Lorimer Moseley on YouTube (the snake bite story is a favorite of mine):
What is a neuromatrix? Essentially, it is a pain map in the brain; a network of neurons spread throughout the brain, none of which deal specifically with pain processing. The way I visualize it is to think about what goes on when you think of your grandmother. There isn’t a grandmother center in the brain, but there are sights and smells (sensory), feelings (emotional awareness), and memories that all come up when you think about her. When we are overwhelmed with pain, those regions become taxed and the individual may have difficulty concentrating, sleeping, and/or may lose his/her temper more easily. Just as each person’s grandmother is different so is a person’s pain and the neuromatrix is affected by past experiences and beliefs.
Pain is an output. It is a response to a threat. When a person is exposed to a threatening situation, biological systems like the sympathetic nervous system, endocrine system, immune system, gastrointestinal system, and motor response system are activated. When a stress response occurs, these systems are either heightened or suppressed to help cope, thanks to the chemicals epinephrine and cortisol.
What is a threat? Threats can take a variety of forms; accidents, falls, diseases, surgeries, emotional trauma, etc. Tissues are influenced by how the individual thinks and feels, in addition to social and environmental factors. The authors propose that when individuals live with chronic pain, their body reacts as though they are under a constant threat. With this constant threat the system reacts and continues to react, and the nervous system is not allowed to return to baseline levels. This can create a patient presentation with immunodeficiency, GI sensitivity, poor motor control, and more. This sounds like most patients who walk into my clinic. The authors suggest that one system may be affected more and that can influence what the patient is diagnosed with even though the underlying biology is the same for many conditions. There are theories for why that happens; genetics, biological memory, or it could be the lens of the provider that the patient sees. There is a table in the article that shows symptoms, diagnosis, and current best evidence treatment for the conditions of fybromyalgia, chronic fatique syndrome, irritable bowel syndrome, and chronic Lyme disease which is worth a look. The treatments all work to calm the central nervous system.
The authors go on to question the relationship between thyroid function and these conditions as changes in cortisol and the hypothalamic-pituitary-adrenal (HPA) axis. The HPA axis is fascinating, and confusing. Luckily, the Pelvic Floor Series Capstone course does a great job breaking it down.
Now that this hypothetical patient is in our treatment room what do we do? The authors suggest seeing these conditions for what they are: chronic pain conditions. They recommend that physical therapists see past the label that a patient may have picked up with a previous diagnosis, and keep the following in mind when treating these patients:
- They are hurting
- They are tired
- They may have lost hope
- They may be disillusioned by the medical community
- They need help
These people need the following from their medical providers:
- Compassion
- Dignity
- Respect
With empathy and understanding therapists can use skills in education, exercise and movement with the intent to improve system function (immune, neural, and endocrine), rather than fixing isolated mechanical deficits.
Louw, Adriaan PT, PhD; Schmidt, Stephen PT ; Zimney, Kory PT, DPT ; Puentedura, Emilio J. PT, DPT, PhD Treat the Patient, Not the Label: A Pain Neuroscience Update.[Editorial] Journal of Women's Health Physical Therapy. 43(2):89-97, April/June 2019.
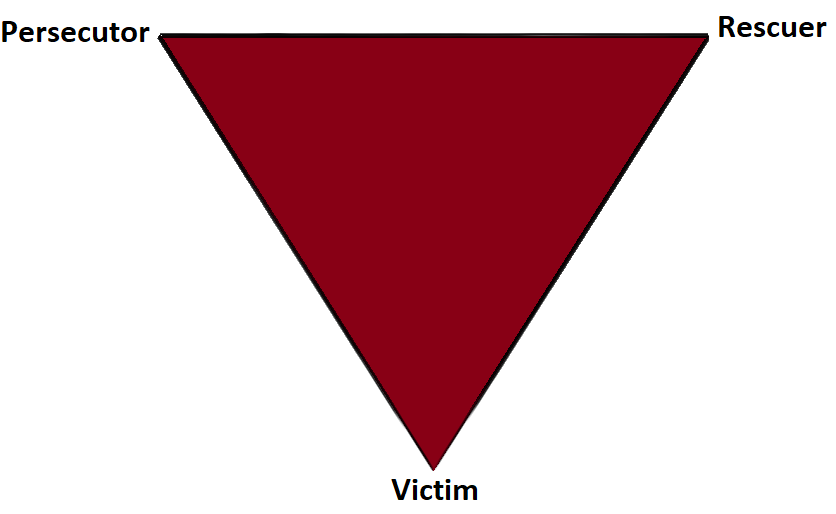
Part 2: The Drama Triangle
This is part two of a three-part series on self-care and preventing practitioner burnout from faculty member Jennafer Vande Vegte, MSPT, BCB-PMD, PRPC. Part One is available here. Jennafer is the co-author and co-instructor of the along with Nari Clemons, PT, PRPC.
Augh, I was so frustrated with myself. I fell for it again. Here’s the scenario: a patient came in suffering excruciating pain. She had been to see a pelvic health professional as well as various medical professionals and was unable to get relief and answers for her rectal pain. She was desperate and called me “her last hope.” Phrases used included, “I need you! Fix me! I hear you are a miracle worker! If you can’t help me no one can!” And just like that I took on the role of Rescuer.
In 1968 a psychiatrist named Stephen Karpman developed a model of personal interaction that he called the Conflict Triangle. It has also become known as the Karpman Triangle, The Drama triangle or the Victim triangle. Per Wikipedia:
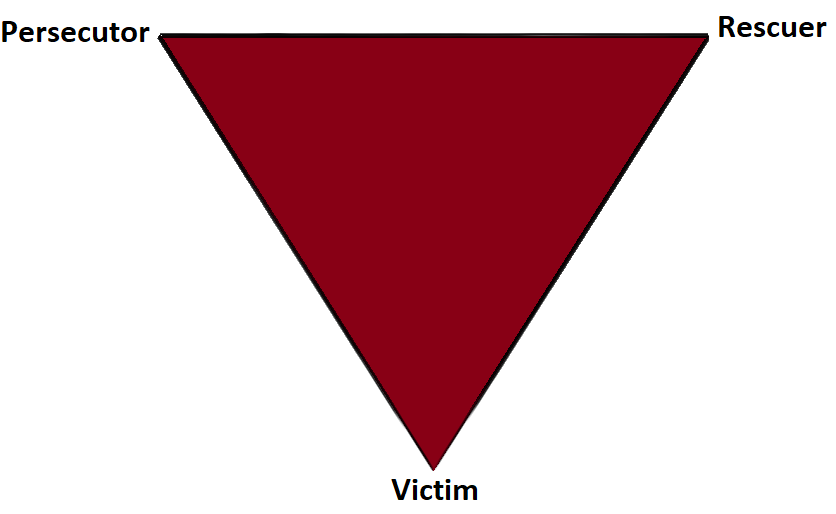
The Victim: The Victim's stance is "Poor me!" The Victim feels oppressed, helpless, hopeless, powerless and ashamed. They seem unable to make decisions, solve problems, take pleasure in life or achieve insight. The Victim, if not being persecuted, will seek out a Persecutor and also a Rescuer who may save the day, but may also perpetuate the Victim's negative feelings.
The Rescuer: The Rescuer's line is "Let me help you." A classic enabler, the Rescuer feels guilty if they don't rush to the rescue. Yet their rescuing has negative effects: It keeps the Victim dependent and gives the Victim permission to fail. The rewards derived from this rescue role are that the focus is taken off of the Rescuer. When they focus their energy on someone else, it enables them to ignore their own anxiety and issues. This rescue role is also pivotal because their actual primary interest is really an avoidance of their own problems disguised as concern for the victim’s needs.
The Persecutor: (a.k.a. Villain) The Persecutor insists, "It's your fault." The Persecutor is controlling, blaming, critical, oppressive, angry, authoritative, rigid, and superior.
 What is interesting about this triangle is that the roles are constantly shifting. In full rescuer mode, I gladly took on this patient, intent on solving her problems. Over time, I saw that my consistent coaching for lifestyle change and self-care was falling on deaf ears. My patient was not following through with anything I asked of her; therefore my treatment plan was not working. The patient began to get frustrated with me. I then cast myself as the victim. She became my persecutor! While perhaps in her mind, I had failed as the rescuer, she was still the victim and I had become her persecutor. At the time, I did not have the skills to know how to navigate this situation in a positive or helpful way. Finally I sought the advice of my supervisor and my therapist to draw up a contract with this patient. The contract outlined each of our responsibilities. If either of us didn’t fulfill our responsibilities, the consequence would be ending our professional relationship. When she persisted, unwilling to do her part, I discharged her per our agreement.
What is interesting about this triangle is that the roles are constantly shifting. In full rescuer mode, I gladly took on this patient, intent on solving her problems. Over time, I saw that my consistent coaching for lifestyle change and self-care was falling on deaf ears. My patient was not following through with anything I asked of her; therefore my treatment plan was not working. The patient began to get frustrated with me. I then cast myself as the victim. She became my persecutor! While perhaps in her mind, I had failed as the rescuer, she was still the victim and I had become her persecutor. At the time, I did not have the skills to know how to navigate this situation in a positive or helpful way. Finally I sought the advice of my supervisor and my therapist to draw up a contract with this patient. The contract outlined each of our responsibilities. If either of us didn’t fulfill our responsibilities, the consequence would be ending our professional relationship. When she persisted, unwilling to do her part, I discharged her per our agreement.
I learned so much from this experience. Here are some things that I have implemented and may be helpful in your practice if you have similar challenges.
- In an initial visit with a new patient I explain that the patient and I make a team and we each have a role to play in reaching the patient’s goals.
- If someone says, “Fix me!” I say, “Think of me as your coach, I can show you how to help your body heal, but it’s your job to do the work.”
- When I hear, “Everyone says you are a miracle worker.” I say, “That is so kind, but it doesn’t work that way. Healing is complicated and everyone has their own journey.”
- In this way, with baby steps, we can get OUT of the drama triangle and into healthy relationships with our patients and the people in our lives.
- Consider the Winner's Triangle published by Acey Choy in 1990.
In her blog NextMeCoaching, Jessica Vader coaches on turning Drama and Control into a Winning situation.
The three roles in the Winner’s Triangle.
Vulnerable – a victim should be encouraged to accept their vulnerability, problem solve, and be more self-aware.
Assertive – a persecutor should be encouraged to ask for what they want, be assertive, but not punishing.
Caring – a rescuer should be encouraged to show concern and be caring, but not over reach and problem solve for others.
If you struggle with professional and personal boundaries, you are not alone, and you can get support. Consider talking with your supervisor, a counselor, reading a good book on the subject, and or taking Boundaries, Mediation and Self Care, a course offering through Herman and Wallace that was designed to help pelvic health professionals stay healthy and inspired while equipping therapists with new tools to share with their patients.
We hope you will join us for Boundaries, Mediation and Self Care this November 9-11, 2019 in San Diego, CA.
Look forward to my next blog where saying no takes an unexpected turn.
The number of individuals who identify as transgender is growing each year. The Williams Institute estimated in 2016 that 0.6% of the U.S. population or roughly 1.4 million people identified as transgender (Flores, 2016). This was a 50% increase from a 2011 survey which estimated only 0.3% or 700,000 people identified as transgender (Gates, 2011). Though these numbers are growing each year, due to increased visibility and social acceptance, it is presumed that these numbers are underreported due to inadequate survey methods, stigma/fear associated with “coming out” and deficient definitions of the multitude of options for gender identity (Flores, 2016).

Though organizations such as WPATH have attempted to standardized care, the patient experience and reception of quality care are significantly lacking. In 2015 the National Center for Transgender Equality performed a groundbreaking survey of 27,215 respondents with the aim to “understand the lives and experiences of transgender people in the United States and the disparities that many transgender people face” (“About,”n.d., para. 1). This survey revealed that 33% of individuals who saw a health care provider had at least one negative experience related to being transgender (National Center for Transgender Equality, 2015). Negative experiences included; being refused treatment, verbal harassment, physically or sexually assault, and teaching the provider about transgender people in order to get appropriate care (National Center for Transgender Equality, 2015). Alternatively, 23% of respondents did not see a doctor when they needed to because of fear of being mistreated as a transgender person (National Center for Transgender Equality, 2015). Though these statistics are staggering and affronting there is hope for a better future.
Research for the care of these patients, specifically related to pelvic floor physical therapy, is on the rise. In the Annals of Plastic Surgery, an article was published with the purpose to capture incidence and severity of pelvic floor dysfunction pre-surgery, monitor any progression of symptoms with standardized outcome measures and highlight the role of physical therapy in the treatment of patients undergoing vaginoplasty (Manrique, et al., 2019). While in the Journal of Obstetrics & Gynecology a retrospective case series similarly focused on physical therapy pre and post-operatively highlighting dilator selection and success, pelvic floor dysfunction including bowel and bladder as well as reported abuse history (Jiang, Gallagher, Burchill, Berli, & Dugi, 2019). Through articles such as these clinicians can expect an uptick in calls questioning if they treat these patients. This begs the question of, "How can you best prepare?"
The answer is simple, attend continuing education. It is where you can not only learn evidence-based evaluation and treatment but also connect with other providers and mentors that care for these patients. In 2020 Herman & Wallace will be offering a continuing education course that serves this exact purpose. Keep your eyes on next years offerings, as spaces will surely fill quickly.
About. (n.d.). Retrieved May 15, 2019, from http://www.ustranssurvey.org/about
Dora Richter. (2019, May 09). Retrieved May 15, 2019, from https://en.wikipedia.org/wiki/Dora_Richter
Jiang, D. D., Gallagher, S., Burchill, L., Berli, J., & Dugi, D. (2019). Implementation of a Pelvic Floor Physical Therapy Program for Transgender Women Undergoing Gender-Affirming Vaginoplasty. Obstetrics & Gynecology,133(5), 1003-1011. doi:10.1097/aog.0000000000003236
Manrique, O. J., Adabi, K., Huang, T. C., Jorge-Martinez, J., Meihofer, L. E., Brassard, P., & Galan, R. (2019). Assessment of Pelvic Floor Anatomy for Male-to-Female Vaginoplasty and the Role of Physical Therapy on Functional and Patient-Reported Outcomes. Annals of Plastic Surgery,82(6), 661-666. doi:10.1097/sap.0000000000001680
National Center for Transgender Equality. (2015). Annual report of the U.S. Transgender Survey. Retrieved May 15, 2019, from https://transequality.org/sites/default/files/docs/usts/USTS-Executive-Summary-Dec17.pdf
Wpath. (n.d.). Standards of Care version 7. Retrieved May 15, 2019, from https://www.wpath.org/publications/soc
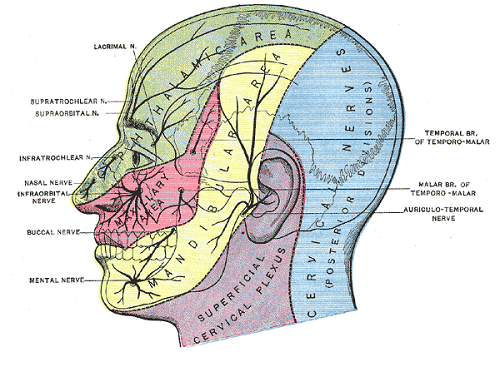
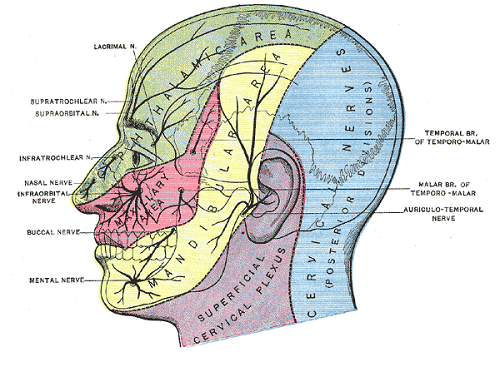
Faculty member Nari Clemons, PT, PRPC recently created a two-course series on the manual assessment and treatment of nerves. The two courses, Lumbar Nerve Manual Assessment and Treatment and Sacral Nerve Manual Assessment and Treatment, are a comprehensive look at the nervous system and the various nerve dysfunctions that can impact pelvic health. The Pelvic Rehab Report caught up with Nari to discuss these new courses and how they will benefit pelvic rehab practitioners.

What is "new" in our understanding of nerves? Are there any recent exciting studies that will be incorporated into this course?
The course is loaded with a potpourri of research regarding nerves and histological and morphological studies. There are some fascinating correlations we see with nerve restrictions, wherever they are in the body. Frequently the nerves are compressed in fascial tunnels or areas of muscular overlap, then the nerve, wherever the location, frequently has local vascular axonal change, which increases the diameter of the nerve and prohibits gliding without pain. This causes local guarding and protective mechanisms. Changing pressure on the nerve can change that axonal swelling and allow gliding without pain.
New pain theory also supports that much of pain perception is the body perceiving danger or injury to a nerve. By clearing up the path of the nerve and mobilizing it, we can decrease the body's perception of nerve entrapment and thus create change in pain levels.
What do you hope practitioners will get out of this series that they can't find anywhere else?
I hope they will leave the course able to treat the nerves of the region, which is essentially the transmission pathway for most pelvic pain. I don't know of other courses that have this emphasis.
You've recently split your nerve course in two. Why the split?
I didn't want this class to be a bunch of nerve theory without the manual intervention to make change. After running the labs in local study groups, we found it took more time for people's hands to learn the language, art, and techniques of nerve work. To truly do the work justice and for participants to have a firm grasp of the manual techniques without being rushed, we found it takes time, and I wanted to honor that, as well as treating enough of the related factors and anatomy to make real and lasting change for patients.
How did you decide to divide up content?
Basically, we divided them up by anatomical origin:
The lumbar course covers the nerves of the lumbar plexus, the abdominal wall when treating diastasis, and treatment of the inguinal canal (obturator nerve, femoral nerve, iliohypogastric, ilioinguinal, genitofemoral nerves). Also, the lumbar nerves have more effect in the anterior hip, anterior pelvis, and abdominal wall.
The sacral nerve course covers all the nerves of the sacral plexus (pudendal, sciatic, gluteal/cluneal, posterior femoral cutaneous, sciatic, and coccygeal nerves), as well as subtle issues in the sacral base and subtle coccyx derangement work as well as the relationship with the uterus and sacrum, to take pressure off the sacral plexus. The sacral nerves have more effect in the posterior and inferior pelvis and into the posterior leg and gluteals.
What are the main stories that either course tells?
Both courses tell the story of getting closer to the root of the pain to make more change in less time. Muscles generally just respond to the message the nerve is sending. Yet, by treating the nerve compression directly, we are getting much closer to the root of the issue and have more lasting results by changing the source of abnormal muscle tone. Rather than an intellectual exercise of discourse on nerves, we devote ourselves to the art of manual therapy to change the restrictions on the pathway of the nerve and in the nerve itself.
If someone went to the old nerve course, what's the next best step for them?
The first course was initially all the lumbar nerves with a dip into the pudendal nerve. They would want to take the sacral nerve course, as those nerves were not covered in the first round.
Anything else you would like to share about these courses?
Sure. Essentially, we will take each nerve and do the following:
- Thoroughly learn the path of the nerve
- Fascially clear the path of the nerve
- Manually lengthen supportive structures and tunnels that surround the nerve.
- Directly mobilize the nerve
- Glide the nerve
- Learn manual local regional integration techniques for the nerve after treatment
- Receive handouts for and practice home program for strengthening and increasing mobility in the path of the nerve
Join Nari at one of the following events to learn valuable evaluation and treatment techniques for sacral and lumbar nerves
Upcoming sacral nerve courses:
Sacral Nerve Manual Assessment and Treatment - Winfield, IL
Oct 11, 2019 - Oct 13, 2019
Sacral Nerve Manual Assessment and Treatment - Tampa, FL
Dec 6, 2019 - Dec 8, 2019
Upcoming lumbar nerve courses:
Lumbar Nerve Manual Assessment and Treatment - Phoenix, AZ
Jan 11, 2019 - Jan 13, 2019
Lumbar Nerve Manual Assessment and Treatment - San Diego, CA
May 3, 2019 - May 5, 2019